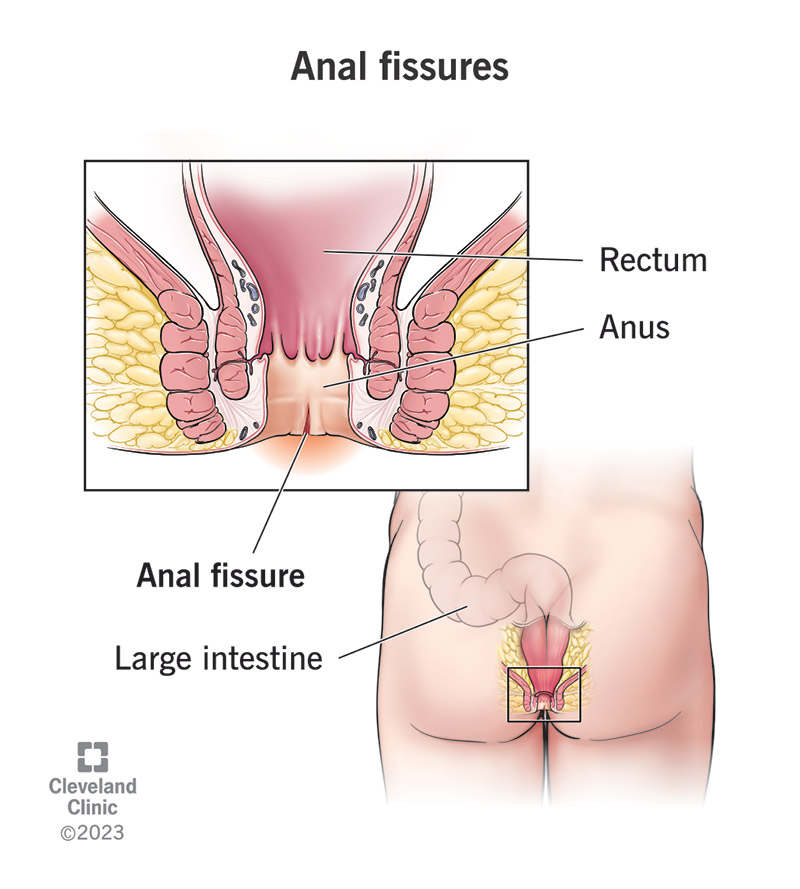
Small rips or cracks in the delicate lining of the anal canal (anal fissures) are a frequent medical problem. Although they may affect persons of any age, they are more common in adults and can be quite painful.
This article’s overarching goal is to educate the reader on anal fissures in as much depth as possible, from the possible origins and symptoms to the available treatment methods.
Few Statistics
- According to research conducted by the American Society of Colon and Rectal Surgeons, anal fissures affect approximately 1 in 20 people at some point in their lives.
- The incidence of anal fissures is higher in adults between the ages of 20 and 50 years.
- Roughly 90% of anal fissures can heal with non-surgical treatments, while the remaining 10% may require surgical intervention (National Institute for Health and Care Excellence).
Causes
Anal fissures can result from various factors, and some of the most common causes include:
- Constipation: Anal fissures are common among those who suffer from persistent constipation. When you strain, you exert extra pressure on the anal canal, which may cause tiny rips.
- Diarrhea: The anal region might get irritated and the skin can become more prone to cracks if diarrhea occurs often.
- Trauma: Traumatizing the anal lining, such as when passing big or hard feces, participating in anal intercourse, or using abrasive toilet paper, may cause fissures to form.
- Anal Spasms: Anal muscle spasms that don’t let up might make it difficult for the fissure to heal, extending the duration of the ailment.
- Inflammatory Bowel Disease (IBD): Chronic inflammation of the digestive system, as seen in Crohn’s disease and ulcerative colitis, may lead to the formation of anal fissures.
Symptoms
Individuals with anal fissures often experience the following symptoms:
- Pain during bowel movements: Anal fissures are characterized by a sharp, searing pain or discomfort during defecating.
- Bright red blood in stools: Anal tissue tears are a typical cause of puddles of fresh blood on the toilet paper or in the bowl.
- Itching and irritation: Due to inflammation, the afflicted region may feel itchy or irritating.
- Muscle spasms: Muscle spasms around the anus, especially if they occur involuntarily, may be quite painful.
Treatment Options
The goals of treating anal fissures are to facilitate healing, reduce discomfort, and stop the injury from happening again. The severity and length of the fissure will determine which of many treatments is most appropriate.
- Self-Care Measures:
- Taking care of one’s anal hygiene by washing with lukewarm water or fragrance-free wipes on a regular basis.
- Adding more fiber to your diet will help you have easier bowel movements by making your stools softer.
- Staying hydrated to prevent constipation.
- Topical Medications:
- Hydrocortisone-containing ointments and lotions are available over the counter to alleviate pain and inflammation.
- Nitroglycerin Ointment:
- The anal sphincter muscle may be relaxed with the use of nitroglycerin ointment, which is available with a doctor’s prescription.
- Calcium Channel Blockers:
- These drugs may lessen the strain on the anal sphincter and increase circulation to speed recovery.
- Botox Injections:
- Botox injections may be used to treat severe instances of anal sphincter spasms by relaxing the muscle and allowing it to recover.
- Surgical Interventions:
- Surgical treatments such as lateral internal sphincterotomy and advancement flap surgery may be explored for fissures that are persistent or are not healing.
When to Seek Medical Assistance
Most anal fissures will heal on their own, however, there are a few cases when you should see a doctor:
- Chronic or severe pain that isn’t helped by over-the-counter pain relievers.
- Large volumes of blood in the feces or other signs of excessive bleeding.
- Self-care attempts not relieving symptoms after more than two weeks.
- Infection symptoms, such as high body temperature, increased edema, or pus drainage from the fissure site.